ADVANCEMENTS IN BATTLING DRUG ADULTERATION
A little while ago I wrote about adulteration of medicines with particular reference to the use of industrial ethylene glycols in children’s cough syrups. This was following my tale of the tragedy in America in 1937 when over 100 people died as a result of taking this Sulfanilamide elixir.
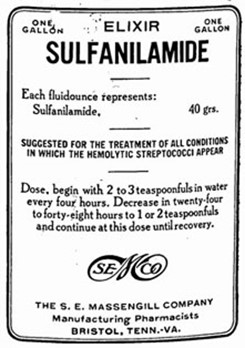
The elixir had been diluted with diethylene glycol but at the time the lack of regulation, never mind safety testing, meant that it was not illegal to market the product (although somewhat ironically the company was found to have mislabelled the product as an elixir when in fact, purely pharmaceutically, it didn’t qualify as such). This mass poisoning of course led directly to the passing by Congress of the 1938 Federal Food, Drug and Cosmetic Act, which required proof of safety before a new medicinal product could be marketed and ultimately led to the FDA as the regulatory body we know today.
The latest tragedy about which I wrote in the previous blog was slightly more sinister as the cough syrups were deliberately produced and distributed with the knowledge that the ingredients were not of the required standard and some 67 deaths resulted. Reports were also received from several African countries of similar deaths associated with other syrups.
The regulatory systems we now have are capable of untangling the web of error and identifying those responsible for the release of the product. As a result, a court in Uzbekistan sentenced 23 people to prison terms over the deaths of those children linked to contaminated cough syrups.
According to a Reuters report the defendants faced jail terms ranging from two to 20 years. They were found guilty of tax evasion, sale of substandard or counterfeit medicines, abuse of office, negligence, forgery, and bribery. An executive director of the local distributors received the lengthiest sentence of twenty years, but of interest is that other jail sentences were handed to officials from the Uzbekistan regulators responsible for licensing imported medicines. In addition to the punitive sentences the court decided that significant compensation would be paid to the families of the children who died.
One cannot help but hope that such salutary punishment will be a real deterrent to others who wish to exploit the sick in this way. However, my recent researches show that the preparation and distribution of such medications is a large, lucrative and growing global business, often involving major criminal syndicates.
The rise of e-commerce makes it easier to obtain medicines online and these may come from unauthorised sources or be adulterated. The World Health Organisation has identified this as a major health challenge for the future and estimates that more than 10% of medicines in low- and middle-income countries are either substandard, adulterated or simply fake! Fortunately, WHO Member States have now formulated a global strategy to tackle these increasingly concerning trends. I wonder if there’s a role for AI here? It might help to reconcile me to its use!
Alas, even AI cannot predict such crimes before they happen, and whilst pharmacovigilance plays its part in post surveillance and the detection of drug adulteration, how about preventative action? As always, public awareness and education is a key factor but sadly, is less accessible in the counties most affected. Timely identification of cases, development of risk management practices, and close partnerships with regulatory authorities leads to increased vigilance, and one would hope that these contributions alongside appropriate punishments at all levels will aid in preventing harm in the future.
